We are learning more every day about how neighborhoods affect not only healthy child development, but also health care usage.
Several studies have linked neighborhood context—measured using the Child Opportunity Index—to preventable emergency department (ED) utilization, hospitalization and hospital readmission among children (Kersten et al. 2018, Krager et al., 2021, Bettenhausen et al., 2022, Ramgopal et al., 2022). One way to measure this preventable health care utilization is by examining ED visits or hospitalizations for “ambulatory care sensitive conditions”—health conditions such as pneumonia or asthma that, with timely and effective primary care, should not normally result in ED visits or hospital admission. For example, Krager et al.'s 2021 study in Pediatrics found that hospitalizations for ambulatory care sensitive conditions are 2.5 times higher for children from very low-opportunity neighborhoods than those from very high-opportunity neighborhoods. Together, these studies suggest that children growing up in very low-opportunity neighborhoods not only are exposed to conditions that increase the risk of illness, but also may lack access to effective primary care, which results in preventable and costly ED visits or hospitalizations. And, when this acute care usage occurs, it can be disruptive for children and their caregivers and sometimes can result in exorbitant financial costs.
A new study examines frequency and resource intensity of emergency department visits
A new Pediatrics study led by Sunitha Kaiser, Associate Professor of Pediatrics at the University of California, San Francisco, provides new insights into how ED utilization differs across children growing up in neighborhoods with different levels of child opportunity. The study uses data from 2018 and 2019 on 6.8 million ED visits by 4 million children at 49 children’s hospitals across the U.S. While previous studies have linked the Child Opportunity Index (COI) to the risk of ED utilization, Kaiser et al. also examine the frequency and resource-intensity of these emergency department visits. Specifically, the authors examine if children visited the ED more than once over the observation period and whether their visits resulted in hospital admission. They also examine whether ED visits were “low resource intensive” (LRI), i.e., visits that did not result in laboratory testing, diagnostic imaging, procedures or medication administration other than ibuprofen or acetaminophen. Low resource intensiveness signals that these visits could have been handled in a primary care or outpatient setting, instead of in the emergency room.
The authors find that ED visits are twice as common among children from very low-opportunity (32%) vs. very high-opportunity (17%) neighborhoods (see Figure 1). As the authors focus on more frequent and low resource intensive visits, these inequities deepen: The percentage of children from very high-opportunity neighborhoods drops, while the percentage of children from very low-opportunity areas rises. Of children with three or more ED visits, 41% are from very low-opportunity and 12% are from very high-opportunity neighborhoods. Having three or more LRI visits is four times more common among children growing up in very low- vs. very high-opportunity neighborhoods.
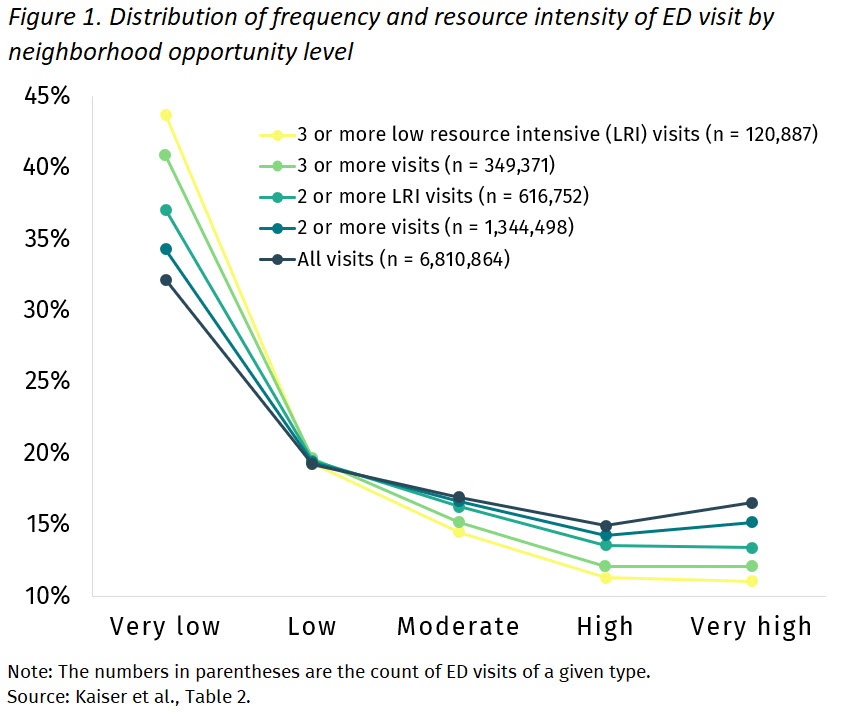
Figure 1 also highlights the distinct disadvantage suffered by children in very low-opportunity neighborhoods. While repeat and LRI visits increase linearly for children from high-, to moderate-, to low-opportunity neighborhoods, there is a much more substantial increase in repeat and LRI visits for children from very low-opportunity neighborhoods. For example, considering children with two or more low resource intensive ED visits, 13% are from very high-, 20% are from low-, but 37% are from very low-opportunity neighborhoods. Children from very low-opportunity neighborhoods account for nearly 40% of these visits, almost twice the percentage for children in low-opportunity neighborhoods.
Lower neighborhood opportunity linked to greater health risks and preventable emergency department visits
Children from lower opportunity neighborhoods are not only more likely to seek medical care in an emergency department, but also to do so for medical issues that should and could be treated more appropriately and more cost effectively in a primary care setting. These findings are consistent with previous studies linking the Child Opportunity Index to ED visits, hospitalizations and hospital readmissions for ambulatory care sensitive conditions. They highlight both the greater health risks and the unequal patterns of health care access and utilization among children growing up in low- and very low-opportunity neighborhoods. They furthermore illustrate that the COI is a powerful predictive tool for health care utilization. The COI could be incorporated into children’s health records because of its prognostic value for preventable health care utilization, and protocols could be developed to assess families’ access to primary care and to connect families with primary care providers in their communities.
The Child Opportunity Index captures many sources of neighborhood disadvantage that individually are known predictors of healthy child development. What’s more, as a composite index, it additionally captures the larger adversity that the accumulation of these multiple sources of disadvantage create. The COI allows us to visualize and measure how residential segregation has led to these multi-faceted inequities in neighborhood opportunity that disrupt families’ access to necessary resources, such as health care. The COI should be considered as a useful data tool for policies and programs aiming to expand health care access in high-need communities and to reduce inequities in access.
Read the full study: Neighborhood Child Opportunity and Emergency Department Utilization
Learn more about the Child Opportunity Index
Explore our library of Impact Stories, including an overview of how the COI is being used to build equity in child health research





